How the latest Obamacare repeal bill would affect New York State

The legislation that Senate Republicans hope to pass next week in a last-ditch effort to dismantle Obamacare would strip away some of the federal funds sent to New York and other states for expanding Medicaid – and give them to the states that didn’t.
The conversion of Affordable Care Act funds into state block grants from 2020 to 2026 is one key part of the bill that Senate Republicans will bring up for a vote by the end of the month, before the expiration of special budget rules that allow passage by a simple majority.
How New York State would be affected
The bill would put the ACA’s financing for subsidized private health insurance and Medicaid expansion into a giant pot and redistribute it among states according to new formulas.
New York would lose $45 billion under the bill’s conversion of Affordable Care Act funds into state block grants from 2020 to 2026, the Avalere consulting firm said.
The Center for Budget and Policy Priorities, a think tank that favors the current health law, said New York State would lose $18.9 billion in 2026 alone.
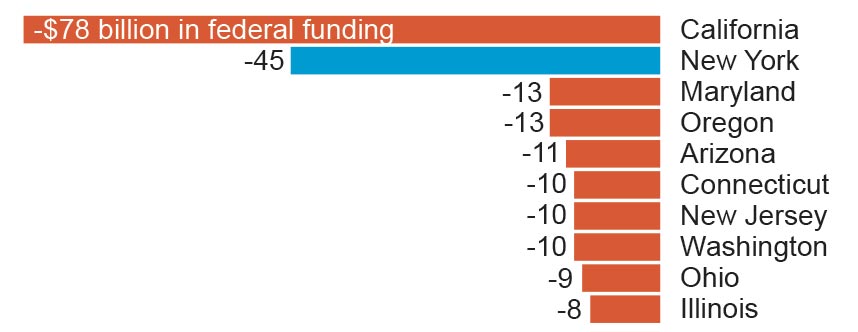
Here’s a look at the 10 states that would lose the most in federal funding if the bill becomes law:
How New York leaders have responded
Supporters of the bill say governors and state legislatures would have broad leeway on how to spend the money, and could also seek federal waivers allowing them to modify insurance market safeguards for consumers. For example, states could let insurers charge higher premiums for older adults.
But with that flexibility also comes the challenge of fixing a broken health care system with less money, a task that New York Gov. Andrew M. Cuomo and at least 10 other governors have publicly rejected.
“I would not trade $19 billion for the flexibility. Because if they cut us $19 billion, if I was as flexible as a Gumby doll, we could not fund our healthcare system,” Cuomo said. “It also puts 2.7 million New Yorkers at risk of losing their health insurance.”
#GrahamCassidy will hurt New Yorkers, who could lose nearly $19 billion in health care funding.
— Kirsten Gillibrand (@SenGillibrand) September 19, 2017
New #Trumpcare would cause millions to lose coverage, eliminates protections for ppl w/ pre-existing conditions & ups out-of-pocket costs.
— Chuck Schumer (@SenSchumer) September 19, 2017
The bill also repeals requirements that individuals buy health insurance and employers offer it, ends subsidies to help people pay premiums, cuts off funding for Medicaid expansion, and makes significant cuts as its reshapes Medicaid.
“They are designed, these cuts, to hurt states that have expanded Medicaid,” Cuomo said. “To penalize us for doing a better job than other states is a gross unfairness.”
Residents of New York and California, which expanded Medicaid and set up insurance marketplaces, had fared better than people living in Texas and Florida, which opted out of both, according to a March 2017 study by the Commonwealth Fund, which studies health issues.
If the bill passes in the Senate, it faces a difficult path in the House, said Rep. Peter King (R-Seaford), who opposes the bill because of the funding cuts for New York.
To penalize us for doing a better job than other states is a gross unfairness.– Gov. Andrew Cuomo
How other states would be affected
The bill would lead to an overall $215 billion cut to states in federal funding for health insurance, through 2026. Reductions would grow over time.
A reduction in federal subsidies for health insurance likely would lead to more people being uninsured, said Caroline Pearson, a senior vice president at Avalere, which specializes in health industry research.
Thirty-four states would see cuts by 2026, while 16 would see increases. Among the losers are several states that were key for President Donald Trump’s election, including Florida, Pennsylvania, Michigan, and Ohio.
California would lose $78 billion, while Texas and Georgia would gain $35 billion and $10 billion, respectively.
“If you’re in a state which has not expanded Medicaid, you’re going to do great,” said Cassidy. “If you’re a state which has expanded Medicaid, we do our best to hold you harmless.”
What else would the bill do?
Named for the bill’s sponsors, Sens. Lindsey Graham (R-S.C.), and Bill Cassidy (R-La.), the bill would repeal much of the Obama-era Affordable Care Act and limit future federal funding for Medicaid. That federal-state health insurance program covers more than 70 million low-income people, ranging from newborns to elderly nursing home residents.
I would not sign Graham-Cassidy if it did not include coverage of pre-existing conditions. It does! A great Bill. Repeal & Replace.
— Donald J. Trump (@realDonaldTrump) September 20, 2017
Independent analysts say the latest Senate Republican bill is likely to leave more people uninsured than the Affordable Care Act, and allow states to make changes that raise costs for people with health problems or pre-existing medical conditions.
The Congressional Budget Office has said it doesn’t have time to complete a full analysis of the impact on coverage before the deadline.
How would Medicaid spending be affected?
Compared to current projected levels, Medicaid spending would be reduced by more than $1 trillion, or 12 percent, from 2020-2036, a study by consulting firm Avalere found. Earlier independent congressional budget analysts said such Medicaid cuts could leave millions more uninsured.
Here’s how else the bill compares

Medicaid expansion
Current: States have the option to expand Medicaid to cover more low-income adults, with the federal government picking up most of the cost.
Senate bill: Ends the federal match for Medicaid’s expansion; ends program’s status as an open-ended entitlement, replacing it with a per-person cap.

Health status-based rates
Current: People cannot be denied coverage due to pre-existing medical problems, nor can they be charged more because of poor health.
Senate bill: Prohibits denying coverage to those with pre-existing condition, but states can seek waivers to let insurers charge more based on health status in some cases.

Subsidies for insurance
Current: Provides income-based subsidies to help with premiums and out-of-pocket costs such as deductibles and copayments; subsidy benchmark tied to mid-level “silver” plans.
Senate bill: Replaces income-based subsidies with block grants to states for health care programs; ends cost-sharing subsidies in 2020.

Standard health benefits
Current: Requires insurers to cover 10 broad “essential services” such as hospitalization, prescriptions, substance abuse treatment, preventive services, maternity and childbirth.
Senate bill: Allows states to seek waivers from the benefits requirement as part of the block grant program.

Coverage mandate
Current: Requires those deemed able to afford coverage to carry a policy or risk fines from the IRS; requires larger employers to offer coverage to full-time workers.
Senate bill: Repeals coverage mandate by removing tax penalty beginning with the 2016 tax year.

Planned Parenthood
Current: Planned Parenthood is eligible for Medicaid reimbursements, but federal money cannot fund abortions.
Senate bill: Planned Parenthood would face a one-year Medicaid funding freeze.
Sources: Department of Health and Human Services, Kaiser Family Foundation
WITH WASHINGTON POST
